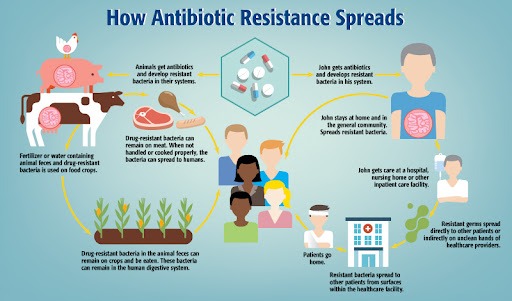
Antibiotic resistance occurs when bacteria evolve mechanisms to survive exposure to the antibiotics designed to kill them. Instead of being destroyed, resistant bacteria continue to multiply, leading to infections that become difficult to treat. It is important to remember that it is the bacteria, not humans, that become resistant. This natural biological process is accelerated by misuse and overuse of antibiotics in humans, animals and agriculture.
How Does Resistance Develop?
Bacteria are remarkable survivors. Their ability to multiply rapidly gives them countless opportunities to mutate. When exposed to antibiotics, most bacteria die, but a few may possess or acquire genetic changes that protect them. These resistant bacteria survive and multiply, passing on their resistance traits to future generations. Resistance spreads in two main ways, Mutation and Horizontal gene transfer. In Mutation, random changes in bacterial DNA give a bacterium the ability to resist an antibiotic. In Horizontal gene transfer, bacteria “swap” resistance genes with one another, even across different species. This makes resistance spread much faster.
Causes of Antibiotic Resistance
Overuse of Antibiotics
Antibiotics are often used when they are not needed. Many people take them for viral infections like flu, colds, sore throat, or COVID-19, where they have no benefit. Self-medication and purchasing antibiotics without a prescription further worsen the problem in many countries. Every unnecessary dose increases the chance of resistance developing.
Misuse in of Antibiotics
Incomplete courses of antibiotics, improper selection of medicine and poor infection-control practices in hospitals give resistant bacteria opportunities to grow. Hospital-acquired infections are now among the most resistant strains.
Use of Antibiotics in Animals and Agriculture
Globally, a large portion of antibiotics is used in livestock. It is not to cure disease, but to promote growth and prevent infections in crowded farms. These antibiotics enter the food chain and environment, encouraging the spread of resistant bacteria to human beings.
Environmental Contamination
Pharmaceutical waste and untreated sewerage containing antibiotic residues create ideal conditions for the development of superbugs. Water sources contaminated with antibiotics expose bacteria to low, constant doses that promote resistance.
Impact of Antibiotic Resistance
Antibiotic resistance threatens every aspect of modern medicine. Without effective antibiotics, routine surgeries, dental procedures, cancer treatments, and organ transplants become dangerous. Simple infections may once again become fatal.Current global estimates reveal that:
- Millions of antibiotic-resistant infections occur each year.
- At least 700,000 people die annually from resistant infections. It is a number projected to rise to 10 million deaths per year by 2050if no action is taken.
- Healthcare costs rise dramatically due to longer hospital stays, more expensive medicines and additional diagnostic tests.
For developing countries, the burden is even greater. Limited access to quality healthcare, lack of proper regulation and widespread over-the-counter antibiotic use create perfect conditions for resistance to spread.
Consequences in Dentistry and Oral Health
Dentists regularly prescribe antibiotics to control or prevent oral infections. However, unnecessary prescriptions, such as for minor pain, routine dental procedures or viral mouth ulcers, add to their resistance. Resistant oral bacteria complicate treatment of periodontal disease, dental abscesses, and post-surgical infections.
With rising resistance, even simple dental extractions or implants carry higher risks. This highlights the importance of strict antibiotic-stewardship protocols in dental practice.
How to control the resistance?
The threat of antibiotic resistance is alarming, but not hopeless. With coordinated efforts at individual, community, national, and global levels, resistance can be slowed and controlled.
1. Use Antibiotics Responsibly
The patients should only take antibiotics prescribed by a qualified doctor & must avoid self-medication and over-the-counter purchases.They must always complete the full course, even if feel better earlier.
2. Strengthen Infection Prevention and Control
Hand hygiene, vaccination, clean water, and improved sanitation help reduce infections, decreasing the need for antibiotics in the first place.
3. Regulate Use in Animals and Agriculture
Countries must implement strict policies limiting antibiotic use in livestock and banning antibiotics for growth promotion. Clean farming practices and improved animal welfare reduce the dependence on antibiotics.
4. Public Awareness and Education
Communities must be educated about the dangers of resistance. Schools, hospitals, dental clinics, and media platforms all play a role in spreading accurate information. Public must realize that Antibiotic resistance is not just a medical issue but a societal problem requiring collective action. The world experienced a golden era of antibiotics, but without urgent changes, we may enter a post-antibiotic age where minor infections become life-threatening once again. Every thoughtful decision, whether by a doctor, a farmer, a policymaker or an ordinary citizen, helps preserve these life-saving medicines. By understanding the problem and acting wisely, we can ensure that antibiotics remain effective for our children, grandchildren, and the generations to come.
Read our full disclaimer.