A healthy smile is built on a strong foundation- the gums and supporting bone that hold your teeth in place. When these supporting tissues become diseased or damaged, even the strongest teeth can become loose or lost. Gums surgery (Periodontal surgery) plays a vital role in restoring the health and stability of these structures. It not only saves teeth but also enhances oral health and aesthetics.
Periodontal Disease
Before discussing surgery, it’s essential to understand periodontal (gum) disease. It is a chronic infection of the gums and bone supporting the teeth. It begins as gingivitis, a mild inflammation of the gums caused by plaque accumulation. If left untreated, it can progress to periodontitis, where the infection extends deeper, causing bone loss and pocket formation around teeth.
Its Common symptoms include:
Bleeding gums during brushing or flossing
Persistent bad breath
Receding gums or “longer-looking” teeth
Loose or shifting teeth
Pus discharge between teeth and gums
When nonsurgical treatments like scaling and deep cleaning fail to control the disease, periodontal surgery becomes the next step.
Periodontal Surgery?
Periodontal surgery is a dental procedure performed to treat advanced gum disease, regenerate lost bone and tissue and improve the function and appearance of the gums. Depending on the severity and type of damage, different surgical techniques are used. These procedures are typically performed by a periodontist — a dentist who specializes in the prevention, diagnosis and treatment of gum diseases.
Purpose of Periodontal Surgery
The main purposes of periodontal surgery include:
Elimination of infection: Removing bacteria and inflamed tissue to halt disease progression.
Reduction of pocket depth: Making it easier to clean around the teeth and prevent reinfection.
Regeneration of lost tissue: Rebuilding bone and ligament destroyed by periodontitis.
Enhancement of aesthetics: Correcting gum recession or uneven gum lines for a better smile.
Facilitation of restorative treatment: Creating a healthy foundation for crowns, bridges or implants.
Types of Periodontal Surgery
It involves a range of procedures tailored to specific conditions.
1. Flap Surgery (Pocket Reduction Surgery)
This is the most common periodontal procedure. The periodontist makes small incisions in the gum to lift a section of tissue, exposing the roots and bone for thorough cleaning. After removing tartar and infected tissue, dentist sutures the gums back in place. It reduces pocket depth, eliminates bacterial infection and facilitates easier home care
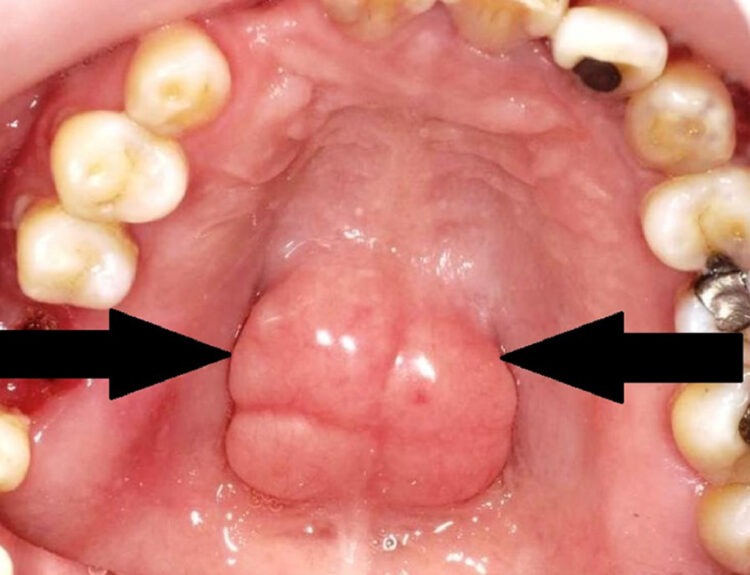
2. Bone Grafting
When periodontitis causes bone loss around teeth, bone grafting helps regenerate the lost bone. Bone from the patient (autograft), donor (allograft) or synthetic material is placed in the affected area. This serves as a scaffold for new bone growth. It restores bone support for teeth and increases stability of loose teeth.
3. Guided Tissue Regeneration (GTR)
In this advanced technique, a special membrane is inserted between the gum and bone to direct the growth of new bone and tissue where needed. The barrier prevents unwanted soft tissue from growing into the area, allowing bone cells to regenerate properly. It encourages natural bone regrowth and prevents further tissue destruction.
4. Soft Tissue Grafting (Gum Graft)
Gum recession can expose tooth roots, leading to sensitivity and aesthetic concerns. In soft tissue grafting, dentist transplant tissue from the palate or another donor source to cover exposed roots or thicken thin gums. It covers exposed roots, reduces sensitivity and improves appearance of the gum line.
5. Crown Lengthening
Dentists perorm this procedure to expose more of the tooth structure either for cosmetic reasons or to allow placement of a dental crown. Small amounts of gum and bone tissue are reshaped to create a balanced gum-to-tooth ratio. It enhances smile aesthetics and facilitates restorative treatments
6. Osseous Surgery
Osseous (bone) surgery is performed to smooth and reshape the bone around teeth after deep cleaning or flap surgery. This helps reduce pockets and allows the gums to reattach more firmly.It improves bone contour and promotes gum reattachment
Post-Surgical Care and Recovery
Proper post-operative care is essential for prompt healing. After surgery, mild discomfort, swelling or bleeding may occur, but these symptoms are temporary and manageable. The patient should
Use prescribed painkillers and antibiotics as directed.
Apply ice packs to reduce swelling.
Eat soft, cool foods for the first few days.
Avoid brushing the surgical area until advised by the dentist.
Rinse with a prescribed antimicrobial mouthwash.
Refrain from smoking, as it delays healing.
The dentist will remove stitches in 1–2 weeks and schedule follow-up visits to monitor healing. With proper care, most patients can resume normal oral hygiene within a few weeks.
Risks and Complications
Although periodontal surgery is safe, like any surgical procedure, it carries some risks, including:
Postoperative infection
Gum recession
Tooth sensitivity
Temporary swelling or bleeding
Rarely, altered tooth alignment or shape of gums
These complications are uncommon and usually be preventable with good post-operative care and regular follow-ups.
Advances in Periodontal Surgery
Advancements in dental technology have made periodontal surgery more predictable and comfortable than ever.
Laser-assisted periodontal therapy (LANAP) uses laser energy to remove diseased tissue with minimal discomfort.
Minimally invasive techniques reduce the need for sutures and promote faster healing.
Biologic agents, such as growth factors and enamel matrix derivatives, stimulate natural regeneration of bone and tissue.
Read our full disclaimer.