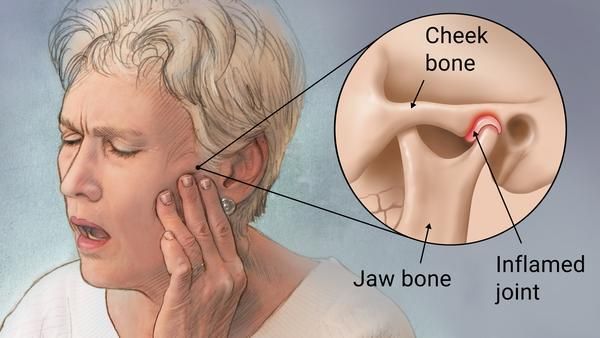
Jaw joint is known as Temporomandibular Joint (TMJ) that acts like a sliding hinge. It connects the lower jaw to the cranium. There is a well-established link between chewing gum and jaw joint pain, also known as Temporomandibular Disorders (TMD). While occasional, moderate gum chewing might not cause issues for everyone, it can be a significant contributing factor or worsen existing TMJ pain. It occurs for several reasons:
Overworking Jaw Muscles: Chewing gum requires repetitive and prolonged use of the jaw muscles, especially the masseter muscles responsible for chewing. This can lead to muscle fatigue, tightness, and even spasms, which are common symptoms of TMD.
Increased Stress on the TMJ: The constant motion of jaw during chewing puts extra strain on the TMJ itself. For individuals with underlying TMJ issues like disc displacement or inflammation, this added stress can exacerbate pain, clicking, popping, and locking of the jaw.
Exacerbating Teeth Grinding: Many people with jaw joint pain also grind or clench their teeth, often unconsciously. Chewing gum can sometimes reinforce this habit, leading to increased pressure on the TMJ and further muscle fatigue.
Uneven Chewing: People generally favor chewing gum on one side of their mouth more than the other. This can create an imbalance in the jaw muscles and joints, potentially contributing to or worsening TMJ symptoms.
Prolonged and Forceful Chewing: Aggressively chewing gum or chewing it for extended periods puts more stress on the jaw joint and muscles compared to eating regular food.
Symptoms of TMD
If you experience any of the following symptoms, and you are a regular gum chewer, it could indicate that gum chewing is contributing to your TMJ issues:
- Jaw pain or tenderness
- Pain in the face, ear, or neck
- Difficulty or pain while chewing
- Clicking, popping, or grating sounds in the jaw joint when opening or closing the mouth
- Locking of the jaw
- Headaches, especially temple headaches
- Toothaches
For accurate diagnosis, your dentist may advise some X-rays;
Dental X-rays to look at your teeth and jaw
CT scan to show detailed images of the bones involved in the joint
MRI to show issues with the joint disk or surrounding soft tissue
Recommendations:
Reduce or eliminate gum chewing: This allows the jaw muscles and joint to rest and recover.
Be mindful of other habits: Avoid other habits that strain the jaw, such as nail-biting, clenching your jaw, or resting your chin on your hand.
Eat softer foods: This reduces the amount of chewing required.
Practice relaxation techniques: Stress can worsen TMJ symptoms, so finding ways to relax can be beneficial.
Treatment Options
Sometimes the symptoms of TMD may subside without treatment. If your symptoms don’t go away, you may require one or more than one of the following at same time;
Medications
Pain killers: If pain medicines available without a prescription aren’t enough to relieve TMJ pain, your dentist may prescribe stronger pain killer for a limited time.
Muscle relaxants. They are sometimes used for a few days or weeks to ease pain caused by TMD that muscle spasms create.
Antidepressants: These medicines are used mostly for depression. But in low doses, they’re sometimes used to ease pain, control bruxism and help with sleeplessness.
Non- Surgical Therapies
Self-care: Apply heat or ice, on the joint, depending on the type of TMJ symptoms. Avoid teeth clenching, gum chewing and nail biting. Rehearse good resting jaw posture with the tongue gently rested on the palate, teeth apart and jaw in a relaxed position.
Oral splints or mouth guards: people with jaw pain will benefit from wearing a soft or firm device inserted over their teeth. The reasons why these devices help are not well understood.
Physical therapy. Along with exercises to stretch and strengthen jaw muscles, treatments might include ultrasound and transcutaneous electrical nerve stimulation, also known as TENS. Also, moist heat and stretching are effective in repeated applications throughout the day.
Surgery
If your condition does not improve and TMD continues, your dentist might refer you to a maxillofacial surgeon for a corrective surgical procedure.
Read our full disclaimer.