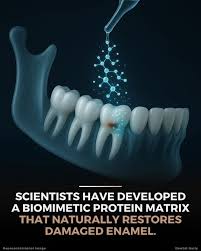
For decades, dentists have repeated the same message that breach of tooth enamel is irreversible. It means that the tooth enamel cannot regrow once it is lost. Enamel is the outermost and hardest layer of a tooth. It is made of tightly packed mineral crystals and contains no living cells. Because of this, unlike bone, it cannot self-repair. When enamel wears away due to acids, sugar, grinding or aging, the damage is permanent. Dentists can only patch or protect the tooth using fillings, crowns or fluoride.
However, in recent years, researchers have been working on ways to naturally rebuild enamel. Among the most promising developments is the creation of a new enamel-hardening protein that can stimulate enamel-like mineral growth on the tooth surface. This innovative protein technology could reshape the future of dental care, offering a biological alternative to synthetic dental restorations.
Tooth enamel is about 96% mineral, primarily hydroxyapatite crystals. This high mineral content makes enamel extremely hard, harder than steel, but also brittle and vulnerable to acid dissolution. Once lost, enamel cannot grow back because it has no living cells. The cells that originally form enamel are ameloblasts. They disappear after tooth eruption. There is no blood supply to deliver the components needed for natural repair. This is why early detection of cavities, fluoride treatments, and preventive dentistry are essential. But what if science could bring enamel-forming ability back?
Need for a New Approach
Current methods like fluoride varnish or remineralizing toothpaste can help strengthen existing enamel, but they cannot rebuild missing areas of the enamel. Dental restorations such as fillings or crowns do the job but are artificial and have a limited lifespan. The idea behind enamel regrowth research is to regenerate enamel biologically, in a way that mimics nature.
New Hardening Protein: How It Works
Researchers have engineered a synthetic or bio-inspired protein that recreates the function of amelogenin; the natural protein responsible for enamel formation during early tooth development. This new protein, in biological tooth repair, acts as a template that can:
bind to the tooth surface
organize ions into an enamel-like structure
guide the growth of new crystals
form a tightly packed mineral layer that resembles natural enamel
Unlike fluoride, which only strengthens surface minerals, this protein works at a deeper structural level, allowing true mineral deposition.
Step-by-Step Mechanism
Application: The protein is applied as a gel, paste, varnish, or solution onto the weakened enamel.
Binding: It attaches itself to the roughened or decalcified enamel surface.
Crystal Nucleation: The protein attracts calcium and phosphate ions from saliva or supplemented solutions.
Crystal Growth: The protein organizes these ions into long, rod-like structures that mimic enamel’s natural crystal orientation.
Layer Formation: Over the period of time, these crystals fuse into a continuous enamel-like layer, increasing hardness and resistance.
In laboratory studies, this process has produced mineral layers that match natural enamel in hardness, thickness, and structure.
Why This Technology Is Revolutionary
If proven successful in human clinical trials, this hardening protein could transform dentistry in several ways:
1. Non-Invasive Treatment for Early Cavities
Instead of drilling and filling, dentists could apply the protein to the early decalcified area, allowing natural enamel-like regrowth.
2. Long-lasting Protection Against Decay
The regenerated enamel layer is harder and more acid-resistant, reducing the risk of recurrent decay.
3. Use in Sensitivity Treatment
Enamel loss exposes dentine, causing sensitivity. Regrowing enamel could seal exposed dentinal tubules more effectively than current desensitizing agents.
4. Potential to Reduce Need for Synthetic Fillings
Biological repairs could decrease dependence on composites, amalgam, or crowns, especially in small lesions.
5. Safer and More Natural Approach
Instead of bonding artificial materials to teeth, this method uses proteins that mimic natural tooth biology.
What Research Says So Far
Different research groups have experimented with enamel-like regrowth using protein-based scaffolds. Though technology varies, most studies show biological tooth repair through;
Promising regrowth within 48 hours to a few weeks
Strong mineral layers up to several micrometers thick
Improved acid resistance compared to untreated enamel
Better bonding between new and old enamel
While these results are exciting, most trials so far involve laboratory models or animal studies. Human trials will be essential to test safety, effectiveness, long-term stability, and ease of use.
Future Applications in Dental Practice
Dentistry may soon include bio-regenerative treatments as routine procedures. Possible future uses include:
1. Enamel Repair Kits at Dental Clinics
Dentists could apply the protein to patients with early enamel defects, white-spot lesions, or post-orthodontic decalcification.
2. At-Home Remineralizing Products
Once safety is established, toothpastes or mouth gels containing the protein may become available for home use.
3. Cosmetic Dentistry
This protein may help repair minor enamel chips, improve smoothness, and increase brightness without harsh bleaching.
4. Pediatric Dentistry
Children with early enamel erosion or developmental defects like hypomineralization could benefit greatly.
Limitations and Challenges
Despite its promise, enzyme-guided enamel regrowth still faces following challenges in biological tooth repair;
Enamel defects larger than a few millimeters may not regrow fully.
Deep cavities still require fillings.
The regrown enamel layer may differ slightly from natural enamel.
Cost and accessibility remain unknown.
Long-term durability must be evaluated.
Read our full disclaimer.