Breast cancer and gum disease may appear to belong to entirely different realms of health. The former is life-threatening and systemic while the latter is localized within the oral cavity. However, emerging scientific evidence suggests that the mouth is not isolated from the rest of the body. Chronic inflammation in the gums may influence systemic health, including the risk and progression of breast cancer. Knowing this connection is important not only for patients but also for healthcare providers who aim to practice comprehensive, preventive care.
Gum Disease
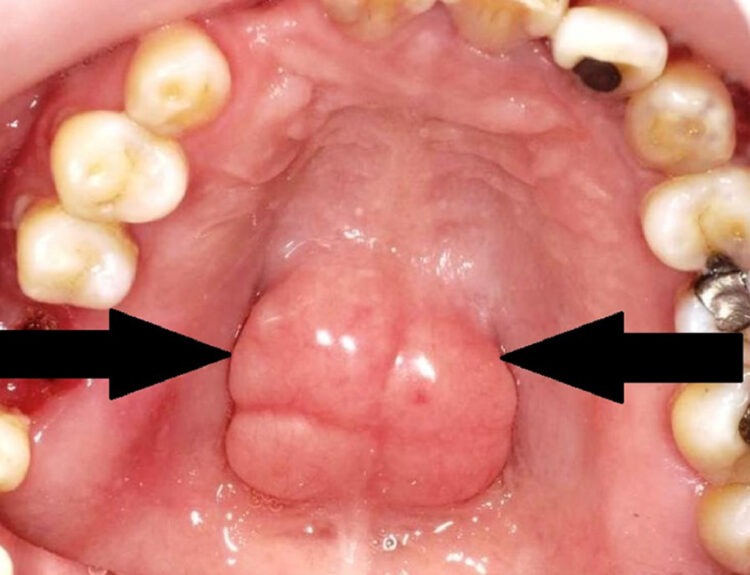
Gum disease is medically known as periodontal disease. It is a chronic inflammatory condition affecting the supporting structures of the teeth. It begins as gingivitis, characterized by redness, swelling and bleeding of the gums. The disease may progress to periodontitis, where there is destruction of the tooth- supporting ligament and jaw bone.
Periodontitis is primarily caused by bacterial accumulation. However, it is not merely a local infection. The inflammatory response of the body to disease causing bacteria results in the release of cytokines and inflammatory mediators such as interleukin-6 (IL-6), tumor necrosis factor-alpha (TNF-α), and C-reactive protein (CRP). These mediators can enter the bloodstream and contribute to systemic inflammation.
Breast Cancer
Breast cancer is the most common cancer among women worldwide. It is influenced by multiple factors, including genetics, hormonal exposure, age, lifestyle, obesity and environmental triggers. Chronic inflammation has increasingly been recognized as a contributing factor in cancer development and progression. Inflammation can promote tumor growth by:
Stimulating cell growth
Inhibiting programmed cell death
Encouraging formation of new blood vessels
Suppressing immune surveillance
This is where the possible link with periodontal disease becomes relevant.
Inflammatory Pathway Connection
Periodontal disease is one of the most common chronic inflammatory conditions globally. Persistent gum inflammation can lead to elevated systemic inflammatory markers. Research has shown that women with chronic periodontitis generally have higher levels of inflammatory indicators in their blood.
Chronic systemic inflammation is known to create a microenvironment that may facilitate tumor development. In breast tissue, inflammatory mediators may contribute to DNA damage, cellular mutations and tumor progression. Therefore, long-standing untreated periodontal disease could theoretically increase susceptibility to cancer development.
Several epidemiological studies have reported an association between a history of periodontal disease and an increased risk of breast cancer. While these studies do not prove causation, they strengthen the hypothesis that chronic oral inflammation may play a role.
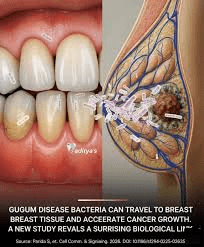
Role of Oral Bacteria
Beyond inflammation, specific gum-disease causing bacteria may also influence cancer risk. Porphyromonas gingivalis and Fusobacterium nucleatum are the bacteria commonly found in advanced gum-disease. They have been found involved in non-oral cancer. These bacteria can:
Alter immune responses
Promote inflammatory signaling pathways
Interfere with normal cell regulation
Enhance tumor cell invasion
Some studies have detected oral bacteria in breast tissue, suggesting that bacterial shifting through the bloodstream may occur. Although research in this area is still evolving, it highlights the systemic implications of oral infections.
Hormonal Factors
Hormonal changes play a central role in both periodontal health and breast cancer risk. Estrogen fluctuations influence gum tissue vascularity and inflammatory responses. Postmenopausal women often experience both increased periodontal breakdown and higher breast cancer risk.
Impact of Cancer Treatment on Oral Health
The relationship between breast cancer and oral health is bidirectional. Treatments for Breast cancer, including chemotherapy, radiotherapy and hormone therapy, can significantly affect oral tissues. Common oral complications include:
Dry mouth
Mucositis
Increased susceptibility to infections
Accelerated periodontal breakdown
Reduced salivary flow alters the oral microbiome and increases plaque accumulation, thereby worsening gum disease. Therefore, breast cancer survivors may require closer dental monitoring.
What Do the Studies Say?
Large cohort studies have suggested a modest but statistically significant increase in breast cancer risk among women with gum disease. For example, some population-based studies have reported up to a 10–15% increased risk in women with chronic periodontitis, particularly among smokers and postmenopausal women. However, it is important to emphasize that:
Association does not equal causation.
Many studies rely on self-reported periodontal status.
Confounding variables may influence outcomes.
Summary
The link between gum disease and breast cancer reflects a broader truth; the human body functions as an interconnected system. Chronic inflammation in one region can influence distant organs. Although current evidence suggests an association rather than direct causation, maintaining good periodontal health is a safe and beneficial strategy with wide-ranging advantages.
For women, especially those in middle and older age groups, prioritizing oral health is not merely about preserving teeth, it may also be part of a comprehensive approach to general well-being.
For women at higher risk of breast cancer, especially those with a family history or genetic predisposition, maintaining optimal periodontal health may be a modifiable preventive factor.
In the future, ongoing research may clarify the precise biological mechanisms connecting periodontal disease and breast cancer. Until then, prevention, awareness, and interdisciplinary collaboration remain key pillars in safeguarding both oral and systemic health.
Read our full disclaimer.