Oro-mandibular dystonia (OMD) is a rare but distressing neurological movement disorder that affects the lower face, jaw, tongue, and sometimes the lips. It causes involuntary, repetitive, or sustained muscle contractions that result in abnormal movements or postures of the mouth and jaw. These spasms may be painful and can interfere with essential functions such as speaking, chewing, and swallowing, profoundly affecting a person’s quality of life. Despite being relatively uncommon, OMD is often misdiagnosed or mistaken for dental, temporomandibular joint (TMJ), or psychological problems, delaying appropriate treatment and care.
Types
Dystonia is a broad term used to describe a group of movement disorders characterized by involuntary muscle contractions. When this condition is localized to the orofacial region, it is referred to as oro-mandibular dystonia. The term “oro” pertains to the mouth, while “mandibular” refers to the lower jaw. These muscle contractions can cause twisting or abnormal movements that make it difficult to perform even simple oral functions.
Primary Dystonia: It is OMD that occurs on its own.
Secondary Dystonia: It occurs as part of a broader neurological condition such as Parkinson’s disease, Wilson’s disease or as a side effect of certain medications, especially neuroleptics used in psychiatric treatments.
Clinically, Oro-Mandibular Dystonia is classified based on the specific muscles involved and the pattern of movement:
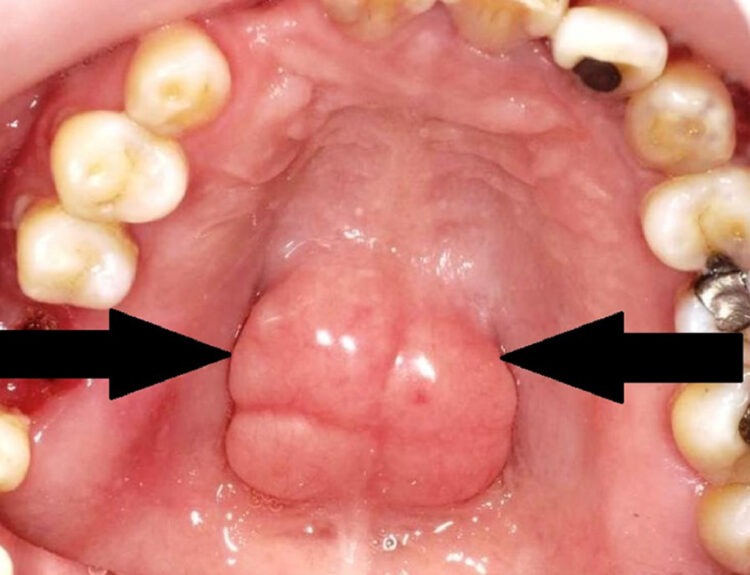
Jaw-Closing Dystonia: The most common type, characterized by excessive contraction of the masseter and temporalis muscles. Patients experience difficulty opening their mouth, clenching of teeth, or even biting their tongue or inner cheeks unintentionally.
Jaw-Opening Dystonia: In this form, the lateral pterygoid and digastric muscles contract involuntarily, causing the mouth to open uncontrollably. This can interfere with speech and make it difficult to keep food in the mouth.
Jaw-Deviating Dystonia: The jaw moves to one side involuntarily due to asymmetric muscle involvement. This deviation can make chewing uneven and lead to facial asymmetry.
Lingual Dystonia: This involves involuntary movements or protrusion of the tongue. It can be particularly disabling, affecting articulation, swallowing and even breathing in severe cases.
Mixed Forms: In many patients, combinations of the above types may occur, making diagnosis and management more complex.
Causes and Risk Factors
The exact cause of OMD is not fully understood. It is believed to result from dysfunction in the basal ganglia. It is the area of the brain that controls and coordinates muscle movements. Abnormal neural signals lead to overactivity of certain muscle groups in the face and jaw.
Several risk factors and triggering conditions have been identified:
Genetic predisposition: Certain forms of dystonia run in families.
Drug-induced OMD: Long-term use of medicines; that help stop nausea,vomiting & motion sickness or medicines used to treat severe mental health conditions like schizophrenia, bipolar disorder, or agitation, can lead to tardive dystonia, a form of secondary dystonia.
Brain injury or stroke: Damage to the basal ganglia or associated neural circuits can lead to dystonic movements.
Peripheral trauma: Dental procedures, ill-fitting dentures, or oral surgeries sometimes precede the onset of OMD, possibly triggering maladaptive neural changes.
Stress and fatigue: Emotional stress or lack of sleep may exacerbate dystonic symptoms.
Clinical Features
The hallmark of OMD is involuntary, repetitive contractions of the facial and jaw muscles. Common symptoms include:
Difficulty in speaking, chewing and swallowing
Uncontrolled jaw movements or clenching
Tongue protrusion or twisting
Facial grimacing
Pain or fatigue in the jaw muscles
Wearing away of teeth due to persistent clenching
Emotional distress and social embarrassment
Interestingly, many patients report a phenomenon known as a “sensory trick” where touching a specific part of the face or chin temporarily alleviates the spasms. Some patients, for instance, lightly touch their lips or hold a toothpick between the teeth reduces the dystonia momentarily.
Impact on Quality of Life
The effects of OMD extend far beyond physical symptoms. Because it interferes with basic oral functions like eating, drinking, and talking. It can lead to malnutrition, weight loss and severe social isolation. Patients often feel embarrassed by their involuntary movements, avoid public speaking, and may even withdraw from social interactions. Chronic pain and frustration can contribute to anxiety and depression, making psychological support an integral part of management.
Diagnosis
Diagnosis can be challenging, as its symptoms mimic several dental and medical conditions. Many patients initially visit dentists, oral surgeons or ENT specialists before being referred to a neurologist. Diagnosis is primarily clinical, based on the characteristic movement patterns and exclusion of other causes. Diagnostic steps include detailed medical and drug history, neurological examination, Electromyography (EMG) to identify abnormal muscle contractions, MRI or CT scan if a structural brain cause is suspected.
Management and Treatment
While there is no definitive cure for OMD, a combination of medical, dental, and therapeutic approaches can significantly reduce symptoms and improve function.
1. Botulinum Toxin Injections
Botulinum toxin (commonly known as Botox) is considered the gold standard for its treatment. It works by blocking the release of acetylcholine at the neuromuscular junction, thereby reducing muscle contractions. The injections are targeted to the overactive muscles, such as the masseter or temporalis, depending on the dystonia type. Relief typically lasts for three to four months, after which repeat injections are required.
2. Medications
Doctors prescribe oral medications in some cases, including Anticholinergics, Benzodiazepines and Muscle relaxants.
However, their effectiveness is variable, and side effects can limit their use.
3. Sensory Tricks and Physical Therapy
Patients are encouraged to identify and use sensory tricks to temporarily reduce spasms. Speech and physical therapy focusing on jaw control, relaxation, and coordination exercises can also help manage symptoms.
4. Dental Appliances
Dentists are the first professionals to encounter Oro-mandibular Dystonia patients due to symptoms like jaw clenching, tooth wear or difficulty in prosthesis adaptation. Custom-made oral appliances or splints help reduce involuntary movements and prevent damage to the teeth or oral tissues. In some cases, adjusting dentures or bite alignment alleviates discomfort.
Recognizing the signs of OMD and referring patients to a neurologist for proper evaluation can lead to earlier diagnosis and management. Collaboration between dental specialists, neurologists, and physiotherapists ensures comprehensive care.
5. Deep Brain Stimulation (DBS)
For severe, drug-resistant cases, neurosurgeons parform deep brain stimulation. It is a surgical procedure that delivers electrical impulses to specific brain regions. It has shown promising results in improving dystonic symptoms.
Read our full disclaimer.