For most people, a root canal is simply a dental procedure that saves a badly decayed or infected tooth. But in recent years, scientists and clinicians have discovered something much more interesting. Treating dental infections through root canal therapy helps people with diabetes control their blood sugar better.
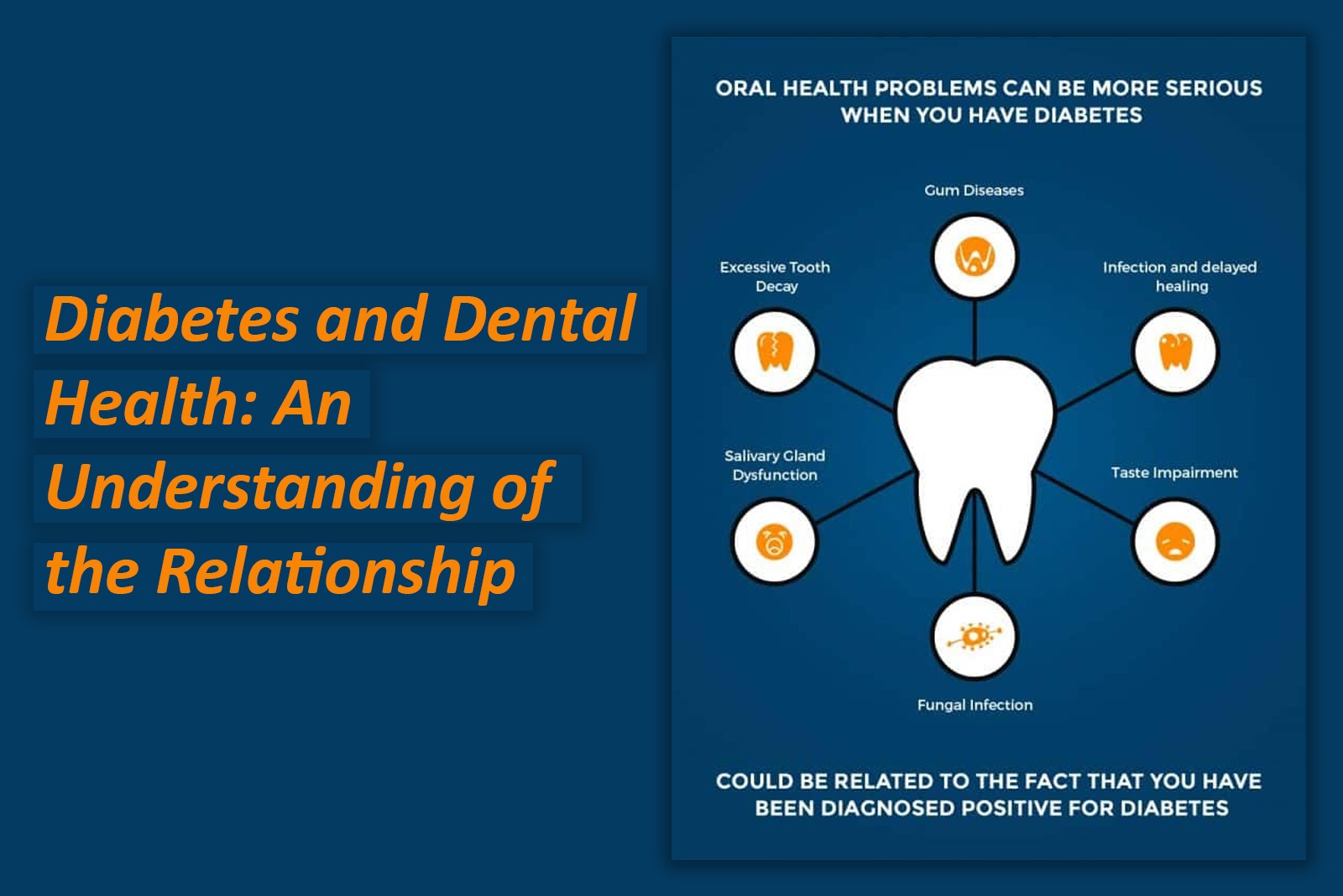
This may sound surprising at first. How can a problem in the mouth affect blood sugar levels? The answer lies in the powerful connection between oral health and the rest of the body. Chronic dental infections increase inflammation, disturb immune responses, and worsen metabolic control. By eliminating these infections, root canal treatment benefits not only oral health but may also support improved diabetic outcomes.
Link Between Dental Infections and Diabetes
The mouth is a gateway to the body. Millions of bacteria live inside the oral cavity, some beneficial and others harmful. When decay reaches the pulp of the tooth, the infection becomes deeper and more severe, leading to Pulpitis or Periapical abscess.
For patients with diabetes, this infection is not just a local dental problem. It has systemic consequences. Chronic infections trigger the body to release inflammatory chemicals such as interleukins and tumor necrosis factor-alpha (TNF-α). These chemicals circulate through the bloodstream and interfere with insulin signaling. As a result, cells respond poorly to insulin and consequently blood glucose levels rise.
Severe dental infections push the body into a state of alert. Stress hormones like cortisol and adrenaline increase to fight the infection. These hormones naturally raise blood sugar levels.Therefore, an untreated dental abscess or infected tooth acts like a constant “stress trigger,” pushing glucose levels higher.
How Root Canal Treatment improve diabetes control
1. Eliminates Chronic Infection
Once the infected pulp is removed, the body no longer needs to fight a constant bacterial threat. As the infection disappears,inflammatory markers decline, immune system stress decreases and overall metabolic function improves. Therefore, diabetics notice better blood sugar stabilization after dental infections are resolved.
2. Reduces Systemic Inflammation
Many studies have shown that patients with Periapical abscess have higher levels of inflammatory cytokines. After root canal treatment;
- CRP (C-reactive protein) levels drop
- insulin sensitivity may improve
- blood glucose becomes easier to regulate
3. Helps Prevent Diabetic Complications
Persistent uncontrolled diabetes leads to following complications
poor wound healing
increased risk of cardiovascular disease
kidney ailments
nerve damage
By controlling oral infections early, RCT contributes indirectly to the prevention of long-term diabetic complications.
4. Improves Eating Ability and Nutrition
A painful, infected tooth makes chewing difficult. Many patients begin avoiding healthy foods like nuts, fruits, or vegetables due to sensitivity. Poor diet can worsen blood sugar control. Once the pain is relieved through a root canal, patients return to a balanced diet that supports diabetes management.
5. Stops the Spread of Infection
If a dental infection or abscess spreads to nearby tissues or bone, the stress on the body increases dramatically. In diabetics, such severity can become medical emergency. RCT helps avoid this risk by addressing the infection before it spreads.
Who Benefits the Most from Root Canal Treatment?
While anyone with an infected tooth needs treatment, certain groups of diabetic patients can experience even greater improvements:
People with poorly controlled diabetes
Patients with repeated gum or dental infections
Older adults with multiple health issues
Individuals with Type 2 diabetes
Root Canal Treatment vs Tooth Extraction: Which Is Better for Diabetics?
Some patients prefer extraction because they fear RCT or believe it is too expensive. However, for diabetic patients, preserving the natural tooth is much better when possible. It not only maintains chewing function but prevents bone loss that occurs after a tooth extraction. This gives long-term oral stability.
On the contrary, extraction may lead to healing delays in diabetic patients and can sometimes increase the risk of infection if not done carefully.
Warning Signs Diabetic Patients Should Not Ignore
Because diabetic patients have a higher risk of complications, even minor symptoms should be taken seriously. These include:
Toothache
Sensitivity to hot or cold
Gum swelling
Pus discharge
Foul taste in the mouth
Darkening of a tooth
Persistent bad breath
Immediate treatment is essential to prevent sudden spikes in blood sugar and diabetes control.
How Diabetic Patients Can Protect Their Oral Health
- Brush twice daily and floss regularly
- Avoid sugary foods and carbonated drinks
- Visit the dentist every 3–6 months
- Monitor for signs of infection
- Maintain good glucose control to improve healing
- Inform your dentist about your diabetes medications and HbA1c levels
Being proactive helps prevent small problems from becoming dangerous ones. A healthy mouth contributes to a healthy body. And for someone living with diabetes, treating tooth infections promptly may make a remarkable difference in long-term health.
Read our full disclaimer.