Dysphagia is a medical term for difficulty in swallowing. It means a person takes more time to move food or liquid from the mouth to the stomach. It is usually associated with neurological disorders, stroke, tumors or systemic diseases. However, most of the people are unaware that oral and dental issues also contribute significantly to swallowing problems. The oral cavity is the gateway to the digestive and respiratory systems; therefore, any alteration in its structure, function or health can affect the ability to chew, prepare food bolus and safely swallow. Dysphagia resulting from dental and oral complications is frequently neglected in clinical discussions, yet it has a profound impact on nutrition, body health, social behavior, and quality of life.
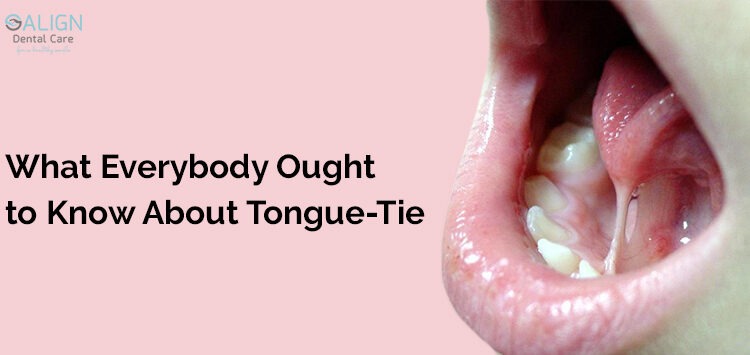
The swallowing process begins in the mouth, where teeth, tongue, salivary glands, gums and oral muscles coordinate to break down food into manageable particles. Proper mastication converts solid food into a soft bolus that can be easily propelled to the throat.
Edentulism
When few or all teeth are missing, chewing becomes difficult. Patients may swallow inadequately chewed food, increasing the risk of choking or aspiration into the lungs. Elderly individuals, people with poor oral hygiene, those with untreated dental diseases or patients wearing ill-fitting dentures are particularly at high risk.
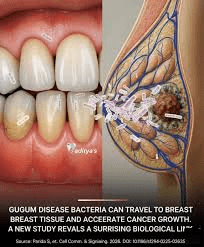
Gum disease and dental infections
They also contribute to swallowing difficulties. Inflamed gums, abscesses, and painful chewing discourage normal eating behavior. Patients chew slowly or avoid chewing on affected sides, leading to asymmetrical muscle activity and altered swallowing mechanics. Chronic infections can spread to surrounding tissues, including muscles involved in swallowing, thereby complicating the condition further.
Xerostomia
Another critical factor is dry mouth, commonly seen in elderly individuals, diabetics, patients undergoing radiotherapy or those taking multiple medications. Saliva is essential for moistening food, facilitating bolus formation, lubricating tissues and initiating digestion. When saliva production decreases, food becomes difficult to manipulate, tends to stick to oral surfaces and swallowing becomes painful and unsafe. Patients with dry mouth frequently complain of choking sensations, difficulty swallowing dry foods like bread or biscuits and prolonged eating time.
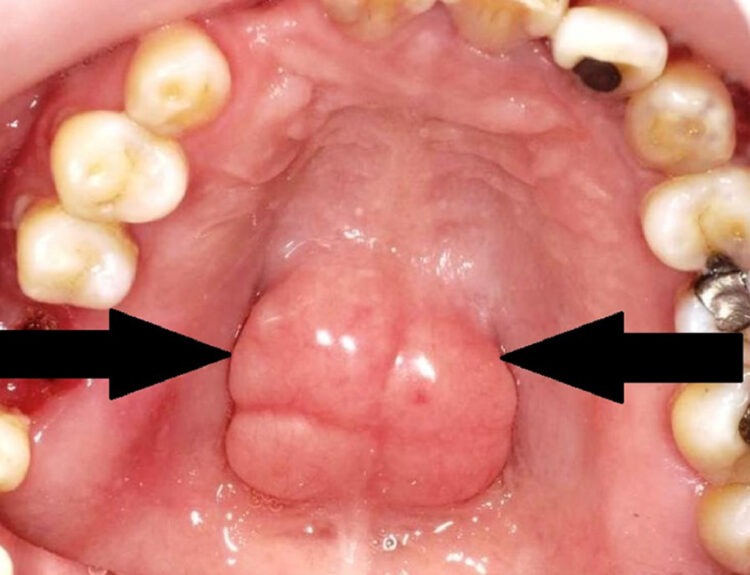
Oral Lesions
Oral ulcers, oral cancers and post-surgical changes can cause painful swallowing. Any lesion in the oral cavity alters tongue movement, chewing strength and swallowing coordination. Patients adopt protective eating behaviors, including skipping meals, preferring liquids only or avoiding chewing altogether. In severe cases, feeding becomes psychologically distressing, affecting mental well-being.
Dentures
Dental prostheses, especially ill-fitting dentures, are another major contributor. Dentures that are loose, unstable or poorly adjusted interfere with chewing movements, tongue space and saliva distribution. Patients may struggle to keep dentures stable while chewing, resulting in ineffective mastication and swallowing difficulty. Some patients fear choking on dislodged dentures, leading to anxiety during meals.
Jaw joint and muscle dysfunction
Muscle disorders of the jaw and temporomandibular joint dysfunction also impair the chewing process. Pain, limited mouth opening, or muscular weakness reduce chewing effectiveness. Similarly, neurological patients with reduced oral motor control experience difficulty coordinating chewing and swallowing, where dental health issues further aggravate the condition.
Psychological issues
Beyond physical problems, dysphagia due to oral issues carries serious nutritional and psychological consequences. People with swallowing difficulty avoid eating in public, withdraw socially and experience embarrassment, frustration or depression. Malnutrition weakens immunity and increases susceptibility to infections, including aspiration pneumonia, which is life-threatening, especially in elderly individuals. In children, untreated dental problems causing dysphagia can impair growth and development, reduce school performance and affect emotional well-being.
Prevention and Treatment
Prevention is the most effective approach. Good oral hygiene, regular dental checkups, timely treatment of dental problems and awareness are essential. Elderly individuals, nursing home residents, stroke patients and those with chronic illnesses must receive special attention. Dentists usually educate caregivers and families about the relationship between oral health and swallowing safety.
Treatment depends on the underlying cause. Restoring missing teeth through dentures, bridges or implants significantly improves chewing and swallowing. Managing gum disease, treating infections, adjusting dentures or addressing oral lesions restores function and comfort. For dry mouth, saliva substitutes, increased hydration, sugar-free chewing gums and medication review may help. Swallowing therapy, dietary modification, physiotherapy for jaw muscles and behavioral counseling complement dental treatment.
Recognizing the role of dental health in swallowing and prioritizing oral care can greatly improve nutrition, health, dignity and quality of life. A healthy mouth is not just about a beautiful smile. It rather, is about survival, comfort and the fundamental human ability to eat and enjoy food safely.
Read our full disclaimer.